Remember how...
Thoracostomy tube placement
 Thoracostomy tube placement is commonly indicated in cases of recurrent pneumothorax or pleural effusions, as well as after thoracic surgery when fluid or air drainage is needed. Tube insertion is usually performed when repeated thoracentesis is required to drain the pleural space; the ultimate goal is the restoration of pleural subatmospheric pressure.
Thoracostomy tube placement is commonly indicated in cases of recurrent pneumothorax or pleural effusions, as well as after thoracic surgery when fluid or air drainage is needed. Tube insertion is usually performed when repeated thoracentesis is required to drain the pleural space; the ultimate goal is the restoration of pleural subatmospheric pressure.
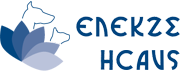
The choice of chest tube size is based on the size of the patient and specifically on the width of the intercostal space and viscosity of the fluid that needs to be drained. A large tube can cause unnecessary pain and patient discomfort, and a very narrow one although suitable for the treatment of pneumothorax, can make the drainage of viscous fluids, such as pus, very difficult. The diameter of the chest tube should approximate that of the principal bronchus and the length should be equal to the distance between the 7th or 8th or 9th and the 2nd rib. Most thoracostomy tubes contain a sharp stylet to aid the puncture of the chest wall (figures 1, 2, 3).
Thoracentesis should be performed prior to anesthesia induction in order to ensure the best possible respiratory function. The best scenario for thoracostomy tube placement is under general anesthesia and concurrent analgesia, but it can also be performed using sedation and local anesthesia (intercostal nerve block and infiltration of the puncture site with local anesthetics), as long as supplementary oxygen is administered.

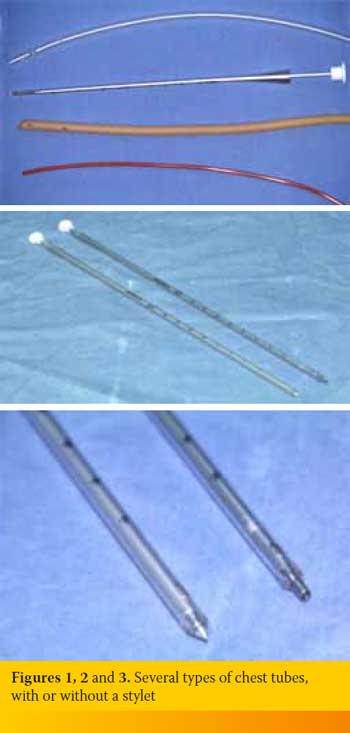
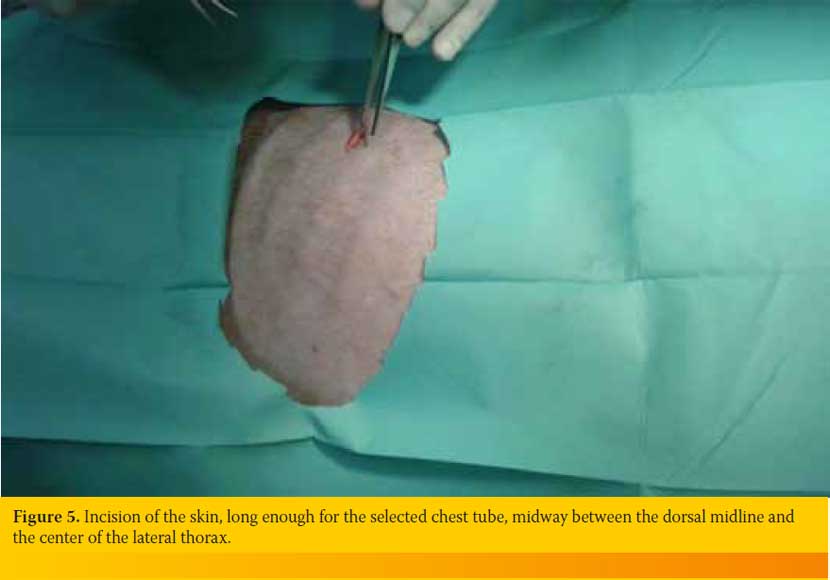
The animal is placed in lateral recumbency, and the chest wall is surgically clipped and scrubbed (figures 4 and 5). Aseptic conditions are maintained throughout the procedure to prevent contamination of the puncture site and/or iatrogenic pyothorax. While an assistant pulls the skin of the thorax cranially, the surgeon identifies the 7th, 8th or 9th intercostal space, and the length of the thoracostomy tube required to reach the 2nd rib is measured and aseptically marked. A small incision of the skin over the chosen intercostal space is made, enough to accommodate the chest tube, midway between the dorsal midline and the center of the lateral thorax (figure 5), and the subcutaneous tissue is bluntly dissected with a hemostat. The stylet of the chest tube is removed and the distal end is clamped off, while the tip of the catheter is held between the tips of a large hemostat (figure 6). The chest wall is punctured by the tips of said hemostat, which are held closed, by gradually applying pressure.
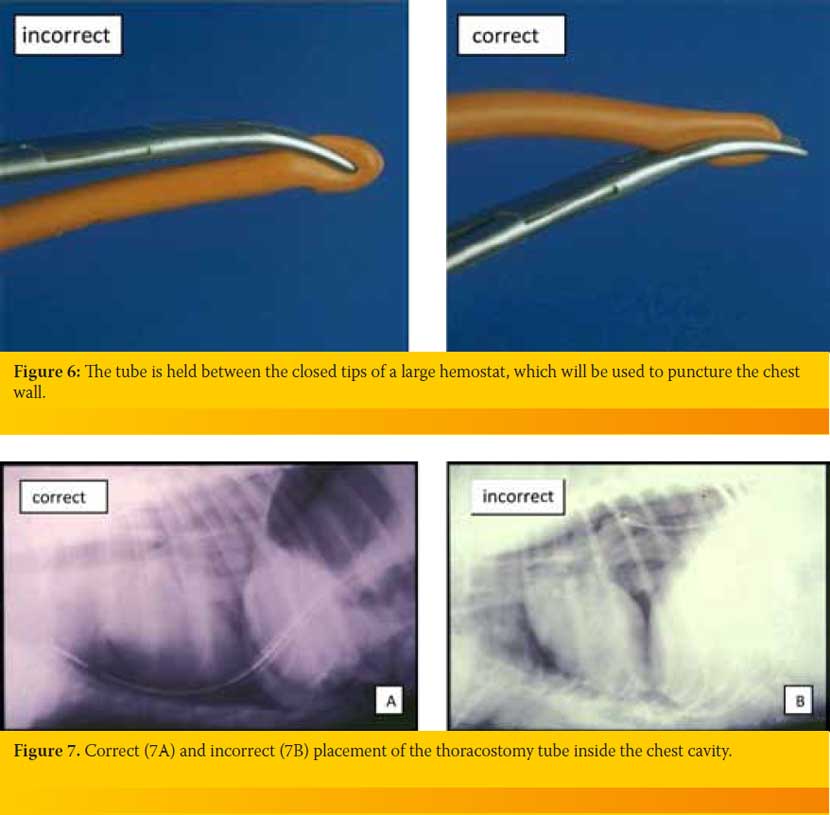
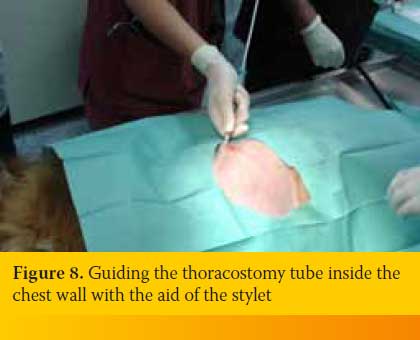 After penetrating the chest wall, the tips of the hemostat are opened and the chest tube is inserted and aimed at the elbow, to allow the tube to move dorsally and toward the 2nd rib (figures 7A and 7B). The stylet of the catheter could be reinserted to aid the guiding of the tube towards the elbow (figure 8), provided that the sharp tip of the stylet is retracted within the tube, in order to avoid injury to the thoracic viscera. After proper placement of the thoracostomy tube, the skin is released to move caudally over the tube, creating a subcutaneous tunnel around it. This tunnel ensures the airtight seal of the site where the tube enters the thoracic cavity, thereby preventing iatrogenic pneumothorax. If no assistant is available to pull the skin, the subcutaneous tunnel can be created by blunt dissection with a hemostat (figure 9), as long as the skin incision is two intercostal spaces caudal to the site where the tube enters the chest cavity.
After penetrating the chest wall, the tips of the hemostat are opened and the chest tube is inserted and aimed at the elbow, to allow the tube to move dorsally and toward the 2nd rib (figures 7A and 7B). The stylet of the catheter could be reinserted to aid the guiding of the tube towards the elbow (figure 8), provided that the sharp tip of the stylet is retracted within the tube, in order to avoid injury to the thoracic viscera. After proper placement of the thoracostomy tube, the skin is released to move caudally over the tube, creating a subcutaneous tunnel around it. This tunnel ensures the airtight seal of the site where the tube enters the thoracic cavity, thereby preventing iatrogenic pneumothorax. If no assistant is available to pull the skin, the subcutaneous tunnel can be created by blunt dissection with a hemostat (figure 9), as long as the skin incision is two intercostal spaces caudal to the site where the tube enters the chest cavity.

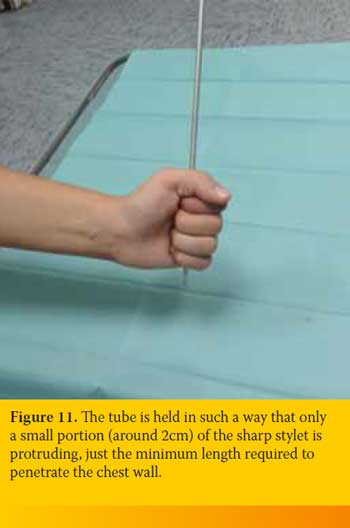
 Another option for inserting the chest tube is to puncture the chest wall using the sharp end of the stylet, after abruptly hitting the blunt end, while holding the tube perpendicular to the chest wall at the chosen intercostal space (figure 10). This technique is not generally recommended as there is a great risk of injuring the intrathoracic viscera, and it is the author’s opinion that it can only be used in large breed dogs. Should this technique be chosen, it is vitally important to leave only a certain, short length of the stylet protruding. This length must be the minimum required to penetrate the chest wall and does not usually exceed 2 cm (figure 11).
Another option for inserting the chest tube is to puncture the chest wall using the sharp end of the stylet, after abruptly hitting the blunt end, while holding the tube perpendicular to the chest wall at the chosen intercostal space (figure 10). This technique is not generally recommended as there is a great risk of injuring the intrathoracic viscera, and it is the author’s opinion that it can only be used in large breed dogs. Should this technique be chosen, it is vitally important to leave only a certain, short length of the stylet protruding. This length must be the minimum required to penetrate the chest wall and does not usually exceed 2 cm (figure 11).
After thoracotomy, the surgeon can easily insert a thoracostomy tube while the whole procedure, taking care not to insert the tube through the thoracotomy but through another intercostal space.
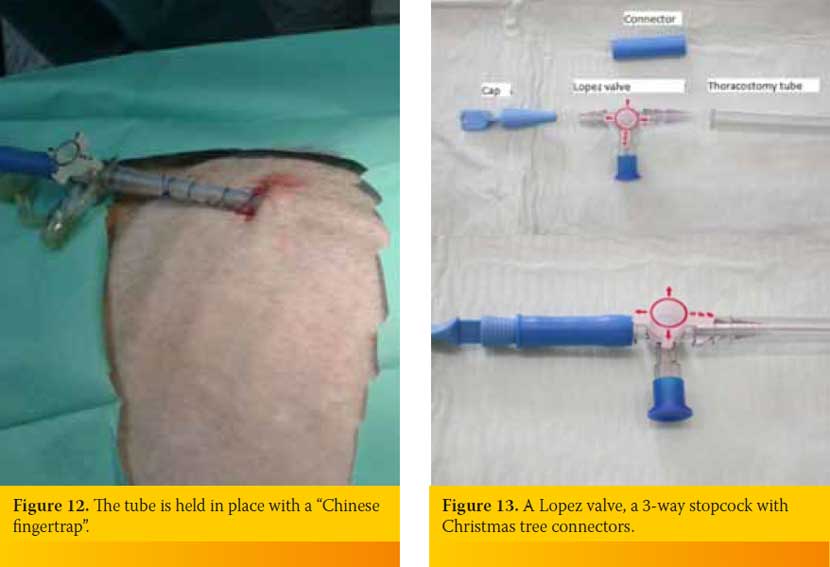
The skin incision is closed with a horizontal mattress suture and the tube is held in place with the use of a “Chinese fingertrap” (figure 12). The site should be covered with an antibiotic ointment and sterile bandages, and an Elizabethan collar should be used.
The chest tube is connected to a Lopez valve, which is a 3-way stopcock with Christmas tree connectors, to minimize the chances of inadvertent dislodgement (figures 12 and 13). Thoracostomy can be used to drain the thoracic cavity by applying negative pressure through the tube, either by manual aspiration using a syringe or with the use of a continuous suction apparatus. The negative pressure applied should not exceed 10-20 cm H2O. Passive drainage can be achieved by either dipping the extension of the thoracostomy tube under the surface of water in a container, or by using a Heimlich valve which allows air to exit the chest cavity during the animal’s exhalation but closes during inhalation. Heimlich valves are suitable for the treatment of mild pneumothorax. The most common reason for their malfunction is occlusion by secretions. For active drainage of the chest cavity, a three-chambered suction apparatus can be used in which the first chamber collects the aspirated fluid, the second chamber acts as a water seal (the tube is submerged under water) to prevent iatrogenic pneumothorax, and the third is filled with 10-20 cm of water to adjust the applied suction pressure.
Bilateral thoracostomy is preferred in massive pleural effusions for optimum drainage of the chest cavity or in cases of pyothorax where lavage is needed.
 Animals with thoracostomy tubes should be monitored continuously for potential dislodgement of the tube or a tube disconnection which will cause immediate pneumothorax. The presence of the tube itself is quite painful and justifies strong analgesia; the most commonly used analgesics include systemic non-steroidal anti-inflammatory drugs and/or opioids, intercostal nerve block of the intercostal space through which the tube enters the chest cavity and the adjacent ones, as well as infusion of local anesthetics in the chest cavity through the thoracostomy tube (commonly after thoracotomy).
Animals with thoracostomy tubes should be monitored continuously for potential dislodgement of the tube or a tube disconnection which will cause immediate pneumothorax. The presence of the tube itself is quite painful and justifies strong analgesia; the most commonly used analgesics include systemic non-steroidal anti-inflammatory drugs and/or opioids, intercostal nerve block of the intercostal space through which the tube enters the chest cavity and the adjacent ones, as well as infusion of local anesthetics in the chest cavity through the thoracostomy tube (commonly after thoracotomy).
The thoracostomy tube can be removed when the fluid production rate falls below 2 ml/kg/24h, a rate that can be attributed solely to the presence of the tube; alternatively, in cases of pneumothorax, it is usually removed after 4-5 days. After removal of the tube, the skin incision must be sutured to prevent iatrogenic pneumothorax, and the intercostal space is left to heal by secondary intention. The surgeon places a new horizontal mattress suture on the skin incision, around the tube, and tightens it at the exact moment that the assistant pulls the tube through. If the tube appears lodged, it is usually due to adhesions to the chest wall, and a small quantity of air or sterile saline should be administered through the tube to help dislodgement.
> References
- Dugdale A. Chest drains and drainage techniques. In Practice 2000, 22:2-15.
- Sigrist NE. Thoracostomy tube placement and drainage. In: Small animal critical care medicine. Silvestein DC, Hopper K (ed). 1st edn. Saunders Elsevier: St. Louis, 2009, pp. 134-137.
- Monnet E. Pleura and pleural space. In: Textbook of small animal surgery. SlatterD(ed). 3rd edn. WB Saunders: Philadelphia, 2003, pp. 387-405.