> Abstract
Rupture of the cranial cruciate ligament is one of the most common canine orthopedic disorders, usually caused by progressive degeneration of unknown etiology. Rarely, it can be caused by trauma, similar to that which occurs in people. Diagnosing this condition requires a detailed history, observation of the dog and physical examination of the stifle joint. Two orthopedic examinations are mandatory: the cranial “drawer” sign and the tibial compression test. Radiographic evaluation of the stifle joint must always be included to differentiate it from other pathological conditions and, also, to receive information regarding the acute or chronic nature of the rupture. Treatment for cranial cruciate ligament rupture can be either conservative or surgical. A number of surgical techniques have been previously described in the literature; however, no study has yet conclusively proven that a single technique is better than any other. Because of this fact, technique selection has been a matter of debate among orthopedic veterinary surgeons.
> Introduction
Cranial cruciate ligament rupture (CrCL) is one of the most frequent orthopedic disorders in dogs and a common cause for lameness due to stifle pathology. The financial costs to dog owners during 2003 in the U.S in regard to all surgical procedures intended for restoration of CrCL rupture were estimated to have reached one billion dollars.1
Even though CrCL rupture can be a result of trauma, it is usually the result of progressive degeneration of the ligament of unknown etiology, leading to partial or complete tear. The consequences of rupture are joint instability, possible tear of the medial meniscus and, eventually, osteoarthritis.
Middle-aged, large breed dogs are those usually afflicted. Newfoundlands, Rottweilers, Labrador Retrievers, American Staffordshire Terriers, Mastiffs and Saint Bernards more commonly present with CrCL rupture. 2
It is possible for 37% of dogs suffering from unilateral CrCL rupture to present with subsequent CrCL rupture in the contralateral limb within 17 months, on average, of the initial diagnosis.3
Treatment for CrCL rupture is either conservative or surgical. The basis for medical treatment is a change of lifestyle, weight loss and non-steroidal anti-inflammatory drug administration. According to one study, medical treatment in dogs weighing less than 15 kg resulted in acceptable limb function in approximately 84-90% of cases. In contrast, lameness improved in only 13% of dogs weighing over 15kg.4 Surgical treatment includes techniques intended for passive stabilization of the joint, such as autograft suturing or nylon sutures, and techniques resulting in dynamic stabilization of the joint, by altering the slope of the tibial plateau in relation to its mechanical axis, or the angle of the patellar ligament in relation to the tibial plateau axis.
Over the last 50 years, an extensive number of surgical techniques have been described; however, they all lack reproducibility.
> Diagnosis
Dogs with CrCL rupture can be classified into two categories. The first includes dogs with an acute onset of complete rupture, whereas dogs with partial rupture belong to the second category.
Dogs with acute and complete rupture present with a history of a sudden onset of moderate to severe lameness, developing suddenly after exercise or in the course of a dog’s normal physical activity.
The highest percentage of large breed and giant breed dogs initially develop partial rupture following a chronic course with moderate lameness. Suddenly, during the dog’s normal physical activity, the partial tear of the ligament becomes complete.
Diagnosing a partial rupture can be challenging. Owners usually report mild lameness in the morning when the dog rises from sleep, which disappears shortly after a few steps and reappears with strenuous exercise. Lameness usually improves following administration of nonsteroidal anti-inflammatory drugs. Eventually, acute deterioration follows due to complete rupture of the CrCL or medial meniscal injury.
Clinical examination includes observation of the animal while walking, or in standing and sitting positions, and also palpation.
Observation of the walking animal helps to assess the grade of lameness and exclude neurologic disorders (instability, ataxia). Sometimes, in the case of a recent CrCL rupture, a characteristic `clicking` sound may be heard when the affected limb is weight bearing. This sound occurs due to compression of the medial meniscus between the medial femoral condyle and the tibial plateau.
Observing the dog in a standing position facilitates evaluation of any anatomical abnormalities in the hindlimbs, such as hyperextension of the stifle and tarsus or genu valgum. These abnormalities are considered to be predisposing factors for CrCL rupture. Observation of the dog in a sitting position or while it is commanded to sit is useful in diagnosing disorders of the stifle and tarsus. If the “sit test” is positive, the presence of abnormal lesions in the stifle or the tarsus joint is almost certain.
In order to perform a “sit test”, the animal is commanded to sit on its hindquarters. A normal dog sits with knees fully flexed; as a result, its hocks approach the ischial tuberosities. Also, the tarsal joints are adequately flexed so that the dog rests on the pubic bones.
In pathological conditions of the stifle or tarsal joint, the dog uses a semi-sitting position in which case the distance between the hock and ischial tuberosity increases or it sits on the non-affected side, by placing all its weight on that hip and keeping the affected limb relatively extended, including both the stifle and tarsal joint (Figure 1).

Palpation is initially performed with the dog in a standing position. Both hindlimbs are palpated simultaneously, in order to detect muscular atrophy, pain, edema or loss of anatomical symmetry. Dogs with chronic rupture of the CrCL present with atrophy in the flexor muscles of the stifle and a palpable enlargement of the synovial capsule in the medial side of the stifle. Subsequently, the dog is positioned in lateral recumbency with the affected limb suspended. Palpation of the stifle joint is performed to detect possible edema or pain, and the position of the patella is evaluated. Afterward, passive range of motion movements of flexion and extension are performed, as well as inward and outward rotation movements and their range and the presence of crepitus are noted. Sometimes, when the stifle joint is extended from the flexed position, a “clicking” sound is heard or felt due to a medial meniscal tear.
The two fundamental diagnostic tests for CrCL rupture are the cranial “drawer” sign and the tibial compression test.
The cranial “drawer” sign must be performed in a sedated or fully anesthetized animal. If this guideline is not observed, false negative results may occur because, due to pain, muscles contract and the joint is temporarily stabilized. False negative results may also be noted in chronic rupture of the CrCL, due to periarticular fibrosis. Positive cranial “drawer” movement is pathognomonic for underlying rupture of the CrCL, even though its absence does not rule out the presence of a rupture.
In order to perform the cranial “drawer” movement test, the joint is held slightly flexed (60o). One hand steadily seizes the peripheral section of the femur, placing the index finger on the patella and the thumb on the lateral fabella. The other hand grasps the central part of the tibia, with the index finger placed on the tibial crest and the thumb behind the head of the fibula.
During this procedure, the angle of flexion and rotation of the stifle must not be altered. While keeping the hand holding the femur steady and consistent, the other hand moves the tibia to a cranial and then caudal direction, in relation to the femur. The test is positive when there is cranial movement of the tibia.
In young dogs, a normal laxity of the joint is observed, resulting in a small range “drawer” movement. In the latter case, “drawer” movement must be compared on both sides, so as to differentiate whether laxity is pathological in one of them.
In cases of partial rupture of the CrCL, the cranial drawer movement of the tibia is quite small (1-2 mm). This finding, combined with a history of pain in the morning following rest and lameness in the limb after intense exercise, constitutes a serious indication of partial rupture of the CrCL.
The tibial compression test can be performed with the dog either in standing position or lateral recumbency. During the procedure, the index finger of the examiner’s one hand is placed on the tibial crest while the thumb and the rest of the fingers hold the peripheral part of the femur. With the other hand, the examiner grasps the metatarsal part of the limb and executes movements of tarsus flexion and extension while keeping the stifle joint stable. If the CrCL has undergone rupture, the examiner can detect a cranial sliding of the tibia in relation to the femur by placing their index finger on the tibial tuberosity. In the case of periarticular fibrosis, false negative results are noted.
In a number of studies, it is mentioned that 20-80 % of dogs with rupture of the CrCL are affected by medial meniscal injuries simultaneously or after a brief time interval.4 The damage is caused by the medial femoral condyle, because each time pressure is applied to the joint during its caudal movement, it compresses and crushes the medial meniscus.
Radiographic diagnosis of CrCL rupture necessitates lateral and caudocranial radiographs of the stifle in a deeply sedated or fully anesthetized dog.
For a lateral projection, the dog is positioned in lateral recumbency on the affected side. The limb is held slightly flexed, or in a neutral position or semi-flexed, and the radiographic beam is centered on the stifle joint. In order to achieve the necessary superimposing of femoral condyles, a radiolucent wedge is placed under the tarsus, so as to slightly elevate the tibia and position it parallel to the radiographic cassette. The other hindlimb is cranially abducted and held in that position.
For a caudocranial projection, the dog is positioned in sternal recumbency, with the affected limb fully extended.
Radiographic findings vary, depending on the chronicity of the CrCL rupture. In lateral radiographs of acute complete rupture cases, a caudal transposition of a radiolucent line is noted, representing the cranial border of adipose tissue located between the fascia of the popliteal muscle and the synovial capsule.5 The transposition of this line is caused by edema of surrounding tissue that causes the caudal translocation of the caudal part of the synovial capsule. Edema in this area also results in loss of radiographic contrast in the area of the infrapatellar fat pad. These radiological findings constitute the earliest signs of complete rupture of the CrCL. (Figure 2).

 In large breed dogs less than 18 months old, rupture of the CrCL is not common, but avulsion fracture from the site of CrCL insertion is a frequent finding. In such cases, a small bone chip appears in the joint; often, a radiolucent area is also visible in the avulsion fracture site. This finding is pathognomonic for avulsion fracture of the CrCL at the site of insertion. (Figure 3).
In large breed dogs less than 18 months old, rupture of the CrCL is not common, but avulsion fracture from the site of CrCL insertion is a frequent finding. In such cases, a small bone chip appears in the joint; often, a radiolucent area is also visible in the avulsion fracture site. This finding is pathognomonic for avulsion fracture of the CrCL at the site of insertion. (Figure 3).
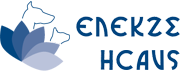
The chronic nature of the disease is the cause for osteoarthritic changes in the joint, mainly featuring osteophyte formation, widening of connective tissue and thickening of the subchondral bone.
During early stages of osteoarthritis, in lateral radiographs, osteophyte formation spreads across the medial and lateral rim of the trochlear groove and on the peripheral border of the patella. During more advanced stages of osteoarthritis, caudocranial radiographs show osteophyte formation in the periphery of the femoral condyles and the periphery of the tibial plateau. During the final stage of osteoarthritis, all joint surfaces are covered with osteophytes (Figure 4).
> Surgical treatment
The classic surgical techniques for restoration of CrCL rupture, also known as “techniques for functional stabilization”, are divided into two categories: intra-articular and extra-articular. The more contemporary techniques, also known as “techniques for geometrical stability”, are intended to modify the inclination angle of the tibial plateau in relation to its mechanical axis or to modify the orientation of the patellar ligament in relation to the tibial plateau following tibial osteotomy.
In intra-articular techniques, stabilization of the joint is accomplished by anatomical replacement of the CrCL by autograft. This category includes the “Over-the-Top” technique, in which autograft from the patellar ligament and the femoral fascia is used6 and the “Under-and-Over” technique, in which autograft from the femoral fascia is used.7 Disadvantages of these techniques lie in the fact that the autograft is often susceptible to ischemic necrosis and rupture and it also has limited tensile strength. 8
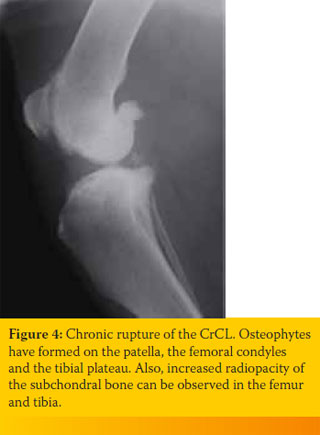
Application of the extra-articular technique began in 1970.9 Nowadays, after several modifications, it is the most frequently used technique compared to all other surgical techniques.
The extra-articular technique provides temporary passive stability to the joint by blocking the craniocaudal and rotary movement of the tibia in relation to the femur until periarticular fibrosis develops, a process completed within 8-10 weeks.
Advantages of the extra-articular technique include its easiness of use, short duration, with good results, a low percentage of complications and low cost. It was attested in a recent study that the percentage of owners who reported being satisfied with the postoperative course of their dog was higher than 90%.10
 In most of the modifications of the extraarticular technique, a non-absorbable synthetic suture is used and it is introduced at the caudal part of the lateral femoral condyle, passing transversely under the patellar ligament and then mediolaterally through a hole drilled in the central part of the tibial tuberosity, eventually to return to the lateral part of the joint, where it is tied to the other end of the suture. The suture is anchored on the femur either by passing around the lateral fabella of the gastrocnemius muscle or directly on the condyle with the aid of a bone anchor (Figure 5).
In most of the modifications of the extraarticular technique, a non-absorbable synthetic suture is used and it is introduced at the caudal part of the lateral femoral condyle, passing transversely under the patellar ligament and then mediolaterally through a hole drilled in the central part of the tibial tuberosity, eventually to return to the lateral part of the joint, where it is tied to the other end of the suture. The suture is anchored on the femur either by passing around the lateral fabella of the gastrocnemius muscle or directly on the condyle with the aid of a bone anchor (Figure 5).
Many modifications of the extra-capsular technique have been described, and they vary depending on suture material and according to the manner of suture anchorage on the bones.
Initially, orthopedic wire was used. Its disadvantage was that in 80% of cases, the wire broke or slid away from the lateral fabella after a period of 4-6 weeks.
Today, nylon suture (leader line, fishing line) or stranded suture of polyethylene (LigaFiba, Fiberwire, OrthoFiber) are employed.
In the case of the nylon suture, five knots are required in order to secure the fastening of the two ends of the suture, thereby creating a sizeable knot that irritates adjacent tissues and causes edema. Metallic cylindrical crimps have been devised to resolve this problem, and are currently in use. After passing both ends of the suture through the crimp, pressure is applied on the crimp so as to secure the suture. The disadvantage of crimps is that the risk of tearing the suture is greater, due to increased loading at the insertion point of the suture into the crimp or due to direct damage of the suture during the application of pressure on the crimp.
The stranded suture of polyethylene is more resilient than its nylon counterpart; it has a smaller diameter, improved resistance to infection and creates a smaller and more stable knot. The appropriate amount of suture tension has not yet been clearly defined.11 However, it has been verified that the tension required during tightening of the suture varies greatly among surgeons. In a recent study, it was noted that the unpredictable postoperative results of the extraarticular technique were mostly the consequence of differentiation in tension applied during suture tightening.12
A recent comparative study between the TPLO and extra-articular technique found no differences in clinical and radiological findings during the postoperative course.13
The major mechanical disadvantage of the classic extra-articular technique is that the anchorage sites of the suture on the bones are non-isometric, signifying that the two ends of the suture do not maintain the same distance throughout the full range of joint movements. As a consequence, the joint’s full range of movement is obstructed, and the suture becomes overloaded.14,15,16
 Due to the fact that stifle joint movements are complicated, there are no specific sites on the femur or the tibia that are absolutely isometric to each other. It has been verified that the anchorage sites of the suture in the classic extracapsular technique located on the caudal part of the condyle at the level of the proximal pole of the lateral fabella (F1), as concerns the femur, and on the tibial tuberosity at the insertion site of the patellar ligament (Τ1), in regard to the tibia, are the least isometric. The sites appearing to be more isometric are the caudal part of the condyle on the level of the distal pole of the lateral fabella (F2) in terms of the femur, and and the caudal wall of the lateral digital extensor muscle groove (Τ3) as concerns the tibia (Figure 6). For suture anchorage at the F2 point, a bone tunnel or bone anchor is required and for the Τ3 point on the tibia, a bone tunnel is necessary. 17
Due to the fact that stifle joint movements are complicated, there are no specific sites on the femur or the tibia that are absolutely isometric to each other. It has been verified that the anchorage sites of the suture in the classic extracapsular technique located on the caudal part of the condyle at the level of the proximal pole of the lateral fabella (F1), as concerns the femur, and on the tibial tuberosity at the insertion site of the patellar ligament (Τ1), in regard to the tibia, are the least isometric. The sites appearing to be more isometric are the caudal part of the condyle on the level of the distal pole of the lateral fabella (F2) in terms of the femur, and and the caudal wall of the lateral digital extensor muscle groove (Τ3) as concerns the tibia (Figure 6). For suture anchorage at the F2 point, a bone tunnel or bone anchor is required and for the Τ3 point on the tibia, a bone tunnel is necessary. 17
A contemporary modification of the extraarticular technique (TightRope) has begun to be employed quite often. With this minimally invasive technique, a flat polyethylene suture tape (FiberTape, Arthrex Inc, Naples FL) is used to connect the femur to the tibia through bone tunnels and anchors on bones with special “buttons”.17 The advantages of this technique concern suture anchorage on nearly isometric sites on the femur and tibia, and the high mechanical endurance of the suture itself. In one study, it was observed that the results of the TightRope technique during the first six months postoperatively did not differ from those of the TPLO.18
From several clinical studies, it emerges that by performing the extra-articular technique, almost 85%-90% of the dogs, depending on the study, presented postoperatively with a normal or almost normal gait.19,20 On the contrary, another prospective clinical study that performed an analysis of limb function by measuring ground reaction forces with the dog on a treadmill, recorded that the percentage of dogs showing improvement after undergoing the extra-articular technique was 40%, and only 14.9% returned to normal function.21
Complications of the extra-articular method are classified as relative to the type of suture or its anchorage technique, joint infection, neurological complications and bandaging and postoperative care.
Tearing or loosening of the suture is included among the complications related to suture material and anchorage technique. The major causes of tearing or loosening of the suture include low mechanical endurance, inflexibility of the suture, high tensile force during tightening, and intense physical activity of the patient during the immediate postoperative period.
These complications can be managed with the selection of a more durable suture material, its anchorage on isometric sites and restriction of the patient’s physical activity in the immediate postoperative period. Infection of the joint is reported in 4% of cases and is characterized by deterioration in lameness and fluid accumulation in the synovial cavity.21 Symptoms usually appear 3-6 weeks postoperatively. Diagnosis is reached by performing an arthrocentesis and collecting synovial fluid samples for analysis and culture.
The most frequent neurological complication is the injury of the peroneal nerve, occurring during suture passage around the lateral fabella.
In order to reduce postoperative edema and pain, the application of cold compresses on the joint is suggested for the first 24 hours. The compresses are applied every six hours and are held on site for 10 minutes. Bandaging the limb for three to five days eases the pain and edema and protects the skin incision from self-trauma. Physical activity must be restricted for a period of four weeks. Thereafter, limited exercise is allowed, which may gradually intensify. After three months, the dog can return to its normal physical activity.

Contemporary studies regarding the surgical management of CrCL rupture have focused on “geometrical stability techniques”. In 1984, Slocum described the cranial tibial closing wedge osteotomy or CTWO.22 The aim of this technique is to reduce or neutralize the force that causes the cranial tibial thrust, exerted during weight bearing of the affected limb. This can be accomplished by decreasing the tibial plateau slope in relation to its mechanical axis, after removing a cranially-based wedge of bone from the proximal tibia. After correction of the tibial plateau slope, when the angle equals 5o in relation to the tibial mechanical axis, the two bone segments are stabilized with a medially applied bone plate (Figure 7).
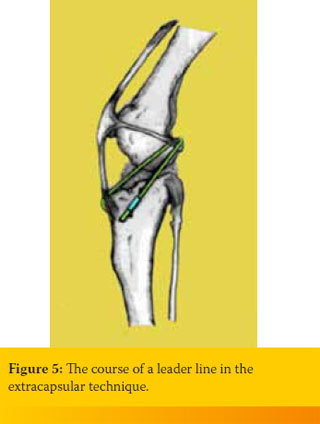
 Shortly after describing the CTWO, the same author described the TPLO technique (tibial plateau leveling osteotomy), which is actually a modification of the former. According to the TPLO, a circular osteotomy is performed on the proximal tibia, followed by rotation of its central part so as to achieve a tibial plateau angle approximately 6.5O in relation to its mechanical axis (Picture 8). Excessive correction of the tibial plateau angle can lead to injury of the caudal cruciate ligament.23
Shortly after describing the CTWO, the same author described the TPLO technique (tibial plateau leveling osteotomy), which is actually a modification of the former. According to the TPLO, a circular osteotomy is performed on the proximal tibia, followed by rotation of its central part so as to achieve a tibial plateau angle approximately 6.5O in relation to its mechanical axis (Picture 8). Excessive correction of the tibial plateau angle can lead to injury of the caudal cruciate ligament.23
To ensure the desired outcome and reduce TPLO complications, the fundamental principles of osteotomy must be adhered to, such as detailed preoperative planning, excellent osteotomy technique, secure stabilization of the two bone fragments that result from the osteotomy, and the rapid return of the dog to its normal activity.
Over the past few years, the technique has undergone certain modifications, enabling it to be used as a contemporary way of restoring patellar luxation and/or limb deformities.24,25
In conclusion, alignment and stabilization of bone segments have been facilitated by the technology of locking screws.26
In 2002, Montavon and Tepic presented a new technique for surgical management of CrCL rupture, which they named ΤΤΑ (tibial tuberosity advancement). This method enables dynamic stabilization of the stifle joint, without the need to alter the tibial plateau angle. 27,28,29
According to TTA, after accomplishing frontal plane osteotomy of the tibial crest and its release from the tibial diaphysis, its cranial advancement is achieved in such a manner that the patellar ligament forms a 90o angle with the tibial plateau. In this way, the cranial tibial thrust force is neutralized and the joint is thus dynamically stabilized.
TTA technique is based upon a mechanical model analysis of the human knee, where it was noted that the resultant of the forces exercised on the knee has a course parallel to the patellar ligament.30 As a result, if the course of the patellar ligament becomes perpendicular to the tibial plateau axis, the resultant force responsible for the cranial tibial thrust will thus be neutralized.
Before performing this technique, preoperative planning is necessary to calculate the exact distance of the tibial tuberosity advancement and to select the proper size for the bone plate.
The common tangent method is used to calculate the distance of tibial tuberosity advancement. According to the latter, a lateral radiograph of the stifle is obtained with the joint almost fully extended. Superimposition of the femoral condyles is necessary. A standardized TTA template with concentric circles (KYON, Zurich, Switzerland) is placed over the radiograph, superimposing on the femoral condyles, in particular; the circle most closely resembling their caudal surface is noted, with attention to the contact points with the tibia. The center of the circle is marked on the radiograph. If the two condyles do not superimpose on the radiograph, the centers of both circles are noted, one for each condyle, medial and lateral, and the middle point of the line connecting these two is also marked. This point is considered to be the center of the circle of the two condyles. To define the center of the circle of the tibial condyles, the template is placed on the radiograph, superimposing on the tibial condyles and their periphery, and the circle that matches the periphery of the condyles is defined. The center of the second circle is marked on the radiograph. The line that connects both centers is drawn. The perpendicular to the line that connects the centers of the two circles, at the same time passing through the contact point of the femur with the tibia, is defined as the common tangent. A line is then drawn, beginning from the cranial margin of the patellar ligament, directed distally and oriented perpendicular to the common tangent. From a point of the line, a perpendicular is drawn that meets the insertion site of the patellar ligament on the tibial crest. The length of this line corresponds to the length of advancement of the tibial tuberosity.31 Finally, another template (KYON), on which bone plates of all sizes are printed, is superimposed on the radiograph to aid in selecting the appropriate size of bone plate required in each case (Figure 9).
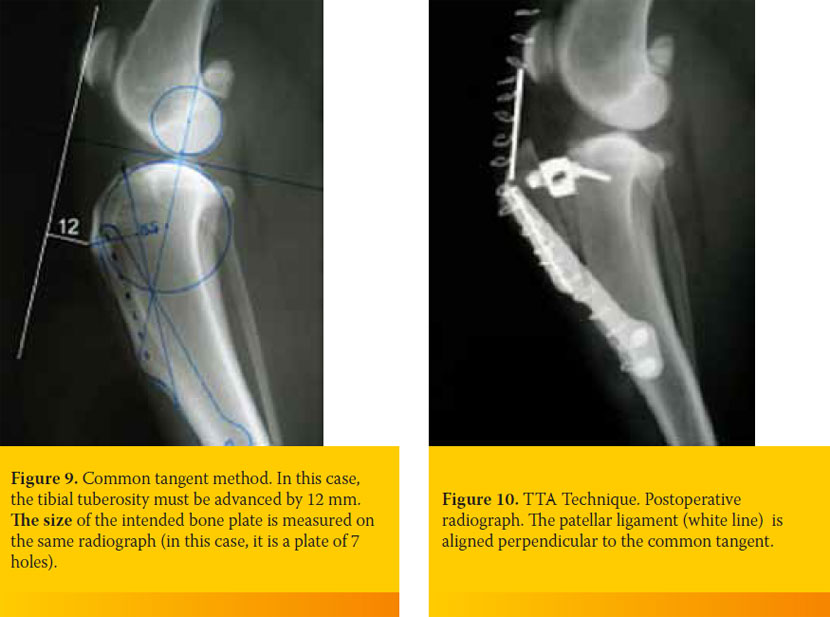
According to the ΤΤΑ technique, a linear osteotomy is performed on the tibial tuberosity.32 A retractor is placed in the proximal part of the osteotomy, with a size equivalent to the length of advancement of the tibial tuberosity. The osteotomized segment of the tibial tuberosity is secured on its new position with a metallic bone plate, located in the medial part of the tibia. In the gap, an autograft of cancellous bone or commercially available bone allograft is inserted, so as to facilitate fracture healing. (Figure 10).
It has been ascertained that ΤΤΑ has a small destructive impact on the contact mechanisms of the stifle joint. Both contact mechanisms of the tibiofemoral and patellofemoral joint are fully restored to normal function after ΤΤΑ. In contrast, the extra-capsular technique and the TPLO technique disturb the points of contact between the articular surfaces, predisposing to the development of osteoarthritis.
The ΤΤΑ technique began to be widely used after 2003. Three studies have been published, concerning its outcome and complications.33,34,35 According to these studies, which included 249 cases of TTA application, the risk of complications ranged from 20% up to 59%. Most of these complications were mild (postoperative edema, bruising). The percentage of serious complications ranged from 12.3% reaching 38% (postoperative meniscal tear, infection, etc.). The percentage of dogs that were readmitted for surgery ranged from 11% to 14%.
> References
1. Wilke VL, Robinson DA, Evans RB, Rothschild MF, Conzemius MG. Estimate of the annual economic impact of treatment of cranial cruciate ligament injury in dogs in the United States. J AM Vet Med Assoc. 2005; 227:1604–7.
2. Duval JM, Budsberg SC, Flo GL, et al. Breed, sex, and body weight as risk factors for rupture of the cranial cruciate ligament in young dogs. J Am Vet Med Assoc 215:811, 1999.
3. Doverspike M, Vasseur PB, Harb MF, et al. Contralateral cranial cruciate ligament rupture: incidence in 114 dogs. J Am Anim Hosp Assoc 29:167, 1993.
4. Vasseur PB. Clinical results following nonoperative management for rupture of cranial cruciate ligament in dogs. Vet Surg .1984:13, 243–246.
5. idmer WR, Buckwalter KA, Braunstein EM, et al: Radiographic and magnetic resonance imaging of the stifle joint in experimental osteoarthritis of dogs. Vet Radiol Ultrasound 35:371, 1994.
6. Arnoczky SP,Trvin GB, Marshalln JL, Saltzman B. The overthe top procedure, a technique for anterior cruciate ligament substitution in the dog, J Am Anim Hosp Assoc 15:283,1979.
7. Shires PK, Hulse DA, Liu W. The under-and-over fascial replacement technique for anterior cruciate ligament substitution in dogs: a retrospective study, J Am Anim Hosp Assoc 20:69-77,1984.
8. Conzemius MG, Evans RB, Besancon MF, Gordon WJ, Horstman CL, Hoefle WD, et al. Effect of surgical technique on limb function after surgery for rupture of the cranial cruciate ligament in dogs. J AM Vet Med Assoc. 2005;226:232–6.
9. DeAngelis M, Lau RE. A lateral retinacular imbrication technique for the surgical correction of anterior cruciate ligament rupture in the dog. J Am Vet Med Assoc 57:79, 1970.
10. Tonks CA, Lewis DD, Pozzi A. A review of extra-articular prosthetic stabilization of the cranial cruciate ligament-deficient stifle. Vet Comp Orthop Traumatol. 2011;24:167–77.
11. Tonks CA, Pozzi A, Ling HY, Lewis DD. The effects of extraarticular suture tension on contact mechanics of the lateral compartment of cadaveric stifles treated with the TightRope CCL or lateral suture technique. Vet Surg. 2010;39:343–9.
12. Dunn AL, Buffa EA, Marchevsky AM, Heller J, Moores AP, Farrell M. Inter- and intra-operator variability associated with extracapsular suture tensioning. An ex vivo study. Vet Comp Orthop Traumatol. 2012;25.
13. Au KK, Gordon-Evans WJ, Dunning D, O’Dell-Anderson KJ, Knap KE, Griffon D, et al. Comparison of short- and longterm function and radiographic osteoarthrosis in dogs after postoperative physical rehabilitation and tibial plateau leveling osteotomy or lateral fabellar suture stabilization. Vet Surg. 2010;39:173–80.
14. Roe SC, Kue J, Gemma J. Isometry of potential suture attachment sites for the cranial cruciate ligament deficient canine stifle. Vet Compar Orthop Trauma. 2008;21:215–220.
15. Hulse D, et al. Determination of isometric points for placement of a lateral suture in treatment of the cranial cruciate ligament deficient stifle. Vet Compar Orthop Trauma .2010;23:163–167.
16. Roe SC, Kue J, Gemma J: Isometry of potential suture attachment sites for the cranial cruciate ligament deficient canine stifle. Vet Comp Orthop Traumatol 21:215, 2008.
17. Cook JL, Luther JK, Beetem J, et al. Clinical comparison of a novel extracapsular stabilization procedure and tibial plateau leveling osteotomy for treatment of cranial cruciate ligament deficiency in dogs. Vet Surg 39:315–23, 2010
18. Moore KW, Read RA. Cranial cruciate ligament rupture in the dog: a retrospective study comparing surgical techniques. Aust Vet J 72:281, 1995.
19. Gambardella PC, Wallace LJ, Cassidy F. Lateral suture technique for management of anterior cruciate ligament rupture in dogs: a retrospective study. J Am Anim Hosp Assoc 31:289, 1985.
20. Conzemius MG, Evans RB, Besancon MF, et al. Effect of surgical technique on limb function after surgery for rupture of the cranial cruciate ligament in dogs. J Am Vet Med Assoc 226:232, 2005.
21. Casale SA, McCarthy RJ. Complications associated with lateral fabellotibial suture surgery for cranial cruciate ligament injury in dogs: 363 cases (1997–2005). J Am Vet Med Assoc 234:229, 2009.
22. Slocum B, Devine T. Cranial tibial wedge osteotomy: a technique for eliminating cranial tibial thrust in cranial cruciate ligament repair. J Am Vet Med Assoc 184:564, 1984.
23. Zachos TA, Arnoczky SP, Lavagnino M, et al. The effect of cranial cruciate ligament insufficiency on caudal cruciate ligament morphology: an experimental study in dogs. Vet Surg 31:596, 2002.
24. Fitzpatrick N, Johnson J, Hayashi K, Girling S, Yeadon R. Tibial plateau leveling and medial opening crescentic osteotomy for treatment of cranial cruciate ligament rupture in dogs with tibia vara. Vet Surg. 2010;39:444–53.
25. Weh JL, Kowaleski MP, Boudrieau RJ. Combination tibial plateau leveling osteotomy and transverse corrective osteotomy of the proximal tibia for the treatment of complex tibial deformities in 12 dogs. Vet Surg. 2011;40:670–86.
26. Conkling AL, Fagin B, Daye RM. Comparison of tibial plateau angle changes after tibial plateau leveling osteotomy fixation with conventional or locking screw technology. Vet Surg. 2010;39:475–81.
27. Montavon PM, Damur DM, Tepic S. Advancement of the tibial tuberosity for the treatment of cranial cruciate deficient canine stifle. In Proceedings of the 1st World Orthopedic Veterinary Congress, Munich, Germany, September 5–8, 2002 (Abstract).
28. Tepic S, Damur DM, Montavon PM: Biomechanics of the stifle joint. In Proceedings of the 1st World Orthopaedic Veterinary Congress, Munich, Germany, September 5–8, 2002 (Abstract).
29. Tepic S, Montavon PM. Is cranial tibial advancement relevant in the cruciate deficient stifle? In Proceedings of the 12th ESVOT Congress, Munich, Germany, September 10–12, 2004 (Abstract).
30. Nisell R, Németh G, Ohlsén H. Joint forces in the extension of the knee: analysis of a mechanical model. Acta Orthop Scand 57:41, 1986.
31. Dennler R, Kipfer NM, Tepic S, Hassig M, Montavon PM. Inclination of the patellar ligament in relation to flexion angle in stifle joints of dogs without degenerative joint disease. Am J Vet Res.. 2006;67:1849–54.
32. Lafaver S, Miller NA, Stubbs WP, et al. Tibial tuberosity advancement for stabilization of the canine cranial cruciate ligament-deficient stifle joint: surgical technique, early results, and complications in 101 dogs. Vet Surg 36:573, 2007.
33. Vezzoni A. Comparison of tibial plateau leveling osteotomy and tibial tuberosity advancement. In Proceedings of the 33rd Annual Conference of the Veterinary Orthopedic Society/2nd Annual World Veterinary Orthopaedic Conference, Keystone, Colo, 2006.
34. Hoffmann DE, Miller JM, Ober CP, et al. Tibial tuberosity advancement in 65 canine stifles. Vet Comp Orthop Traumatol 19:219, 2006.
35. Lafaver S, Miller NA, Stubbs WP, et al. Tibial tuberosity advancement for stabilization of the canine cranial cruciate ligament-deficient stifle joint: surgical technique, early results, and complications in 101 dogs. Vet Surg 36:573, 2007.
36. Stein S, Schmoekel H. Short-term and eight to 12 months results of a tibial tuberosity advancement as treatment of canine cranial cruciate ligament damage. J Small Anim Pract 49:398, 2008.